How decrease inequalities in cancer therapeutics/care and prevention?
Conference organised by the Pontifical Academy of Sciences and the European Academy of Cancer Sciences

Tomorrow, Friday 24 February 2023, at 11.30 a.m. in the Sala Marconi (Palazzo Pio – Piazza Pia, 3 – Rome) the Press Conference on the Conference Strategies to decrease inequalities in cancer therapeutics/care and prevention, organised by the Pontifical Academy of Sciences and the European Academy of Cancer Sciences (Vatican – Casina Pio IV, 23-24 February 2023) will take place
The presentation will be attended by:
– His Eminence Card. Peter K.A. TURKSON, Chancellor of the Pontifical Academy of Sciences;
– Joachim VON BRAUN, President of the same Academy;
– Laura AMBROSINO;
– Mammen CHANDY;
– Douglas LOWY.
Accreditation procedures for the press:
Journalists and media practitioners wishing to attend must send a request, by Friday 24 February 2023 at 9:00 a.m., through the Holy See Press Office’s Online Accreditation System at: press.vatican.va/accreditations
Concept of the Conference
Inequalities tend to be systemic and often entrenched in socio-economic and political structures within and across countries. In recent years, analyses of inequalities related to cancer therapeutics/care and prevention have shown important disparities between and within countries, including those with high economic standards. The conference will explore how to overcome disparities even in the present relatively unequal financial situation between countries.
Over the last decades, the impressive development of basic and technological research has offered unexpected clinical/prevention research opportunities. Still, the translation to cancer therapeutics/care and prevention is severely hindered by the sub-optimal structuring underpinning of clinical and prevention research necessary to develop personalized/precision cancer medicine. This situation has
been the subject of several investigations in Europe. Lately, a collective attempt to overcome some of these problems has materialised with the launching by the European Commission of the Cancer Mission and the Europe´s Beating Cancer Plan. The EU should further explore opportunities to engage in international scientific collaborations and action partnerships to reduce related inequalities. The US
Moonshot initiative is an illuminating example attempting to bridge basic and clinical cancer research.
The conference will address some of the important factors behind inequalities and how to improve equal access to cancer therapeutics/care, diagnostics and prevention. The European Union (EU) and its Member States’ efforts are timely and of global interest. However, the success of these efforts will heavily depend on the strategies used to invigorate and interconnect the complete cancer research continuum. The conference will also address cancer therapeutics/care and prevention internationally, including low-income countries.
Translational research bridges the gaps in the cancer research continuum from basic to clinical/prevention research and further to implementation and follow-up to assess effectiveness. Several gaps need to be bridged to achieve a coherent research continuum, and Comprehensive Cancer Centers (CCCs) and networks thereof constitute essential infrastructures for integrating therapeutics/care,
prevention, research and education. The organisational complexity of the infrastructures needed to develop innovative treatments for the many subgroups of patients and individuals at risk poses major challenges, with the critical mass of patients, biological materials, technological resources and competencies as limiting factors. Structuring translational cancer research for all therapeutics/care and prevention components is necessary to achieve effective international innovation and decrease present inequalities.
New knowledge is acquired much faster in the basic and technological research areas than in clinical and prevention cancer research. This is exemplified by the fact that translational research is often referred to as crossing “the valley of death”, the large gap between basic research and translation to novel therapeutics. It is also illustrated by the concept of “P4 medicine” relevant for chronic diseases with cancer among them: cancer medicine should be “Preventive, Predictive, Personalized and Participative”, but it is not.
Basic and technological research sets the agenda for innovation of clinical and prevention translational cancer research aimed at personalized/precision cancer medicine. A coherent bridging of basic and preclinical research and its integration with early clinical trials, is a primary responsibility for countries with well-developed basic research. Effective translational research covering late clinical, outcomes and
health economics requires high-quality geographically spread infrastructures with good access to local patient populations. These facilities can boost expertise and enable capacity building, especially in underprivileged areas. The establishment of suboptimal infrastructures for research will rather aggravate than mitigate inequalities.
There is a good reason for the initiation of two comprehensive strategies, the Moonshot in the US and the Mission on Cancer in Europe. Despite advances made in cancer research over decades, the cancer problem is still increasing, both in incidence, prevalence and the number of patients dying from it. Expanding possibilities for both prevention and therapeutics are expected to come from basic/technological research. However, establishing a coherent and effective translational research continuum is a major challenge due to the complexity to effectively exploit the increasing number of promising innovations from basic research.
Cancer biology research is expected to provide new information on causes of cancer, relevant targets for early detection, identification of new tumour cell vulnerabilities, molecular pathology and stratification of patients for treatment, and rational combinations of anticancer agents paving the way for preclinical research.
Immunology research will lead to new insights to further develop immuno-oncology – immunecheckpoint inhibition, adoptive T-cell therapy, neoepitopes as targets for vaccination strategies, and the microbiome for immunomodulation.
Technological research will innovate diagnostics through new imaging technologies, radiation therapy, surgical and endoscopic advances, new developments in digitized pathology through omics and IT technologies, and digital data collection.
Data sciences will boost clinical and prevention research through computational approaches, including bioinformatics, modelling, systems and computational cancer biology, diagnostics, clinical trials and outcomes research.
A long-term goal is the structuring cancer activities in the EU member states to improve multidisciplinary treatment/care, prevention and research. Currently, personalized/precision cancer medicine development is impossible without strong infrastructure support, which cannot be established in each centre. Sharing advanced infrastructures is mandatory both within and between countries. Access to sufficient numbers of patients, once stratification technologies for treatment will be more advanced, will further force international collaborations. With this perspective, each member state has to plan the implementation of Europe´s Beating Cancer Plan, and the Mission on Cancer. The latter focusing on innovation, has to facilitate international research collaboration to establish a coherent cancer research continuum representing all therapeutics/care and prevention components.
A Comprehensive Cancer Center (CCC), as defined by the Organisation of European Cancer Institutes and the German Cancer Aid, should be established in each member state and in countries with large populations, preferentially with one CCC per 5 million inhabitants. To reach all patients, the CCCs have to assure that cancer patients in their surrounding geographic areas have access to the same high level of cancer care andinvolving clinical cancer centres and hospitals in research collaborations and education. Comprehensiveness means integrating cancer therapeutics/care, prevention, research and education to secure continuous innovation. For each country, research priorities should be defined and supported by the necessary infrastructures.
Presentations will discuss the concept of CCC and the implementation of translational research to develop personalized/precision cancer medicine in selected EU member states with focusing on infrastructures, as described at the European Cancer Research Summit in Porto, in May 2020. Examples of circumstances in other continents like Asia, Africa and Australia will be presented. The discussion will focus on the need for educational support, the expected difficulties and barriers.
An important goal of both Europe´s Beating Cancer Plan and the Mission on Cancer is the reduction of present inequalities. Innovative translational research needs to be embedded in well-functioning healthcare and prevention organisations that foster new types of collaborations to achieve the necessary critical mass, a driving force towards international research collaborations. All components of
therapeutics/care and prevention should be targets for research. To achieve sustainability, long-term support for CCCs and collaboration between CCCs are mandatory. Consortia of CCCs should collaborate with basic/preclinical research centres and research-oriented hospitals. Sharing the most advanced infrastructures will support innovative research in the EU member states and help decrease inequalities between and within countries. Cancer Core Europe and Cancer Prevention Europe may serve as examples.
The number of consortia has to expand to cover the cancer research continuum properly. The clinical trials methodologies show increasing complexity from proof-of-concept clinical trials to next-generation clinical trials, clinical-practice changing trials and implementation research. Thus, different geometries regarding collaborations need to be explored. Consortia will be indispensable for the various components of prevention, immunotherapy, radiation therapy, innovative surgery, health-related quality of life research, outcomes research, health economics etc. Paediatric oncology is already organised in this way, but geriatric oncology is not.
Mitigating inequalities will also need the linking with insights into the economic consequences by outcomes research and health economics analyses. It is often more cost-effective to prevent than treat diseases, and treatment at an early stage of the disease is often more effective than at later stages. The basic idea of personalized/precision cancer medicine is “the right treatment for the right patient at the right time” to avoid unnecessary treatments and side effects. A stronger focus on the definition of evidence-based medicine, including survival and health-related quality of life, should lead to a decrease of treatments that lack sufficient evidence.
Related

“Being Catholic in Tanzania is a source of pride”
Fundación CARF
16 April, 2025
6 min

The Vatican Suppresses the Sodalitium of Christian Life After a Long Discernment Process
Exaudi Staff
15 April, 2025
1 min

From Kahlenberg to the Papal Cross – Polish Night Way of the Cross in Vienna
Heschel Centre for Catholic-Jewish Relations at the Catholic University of Lublin
15 April, 2025
2 min
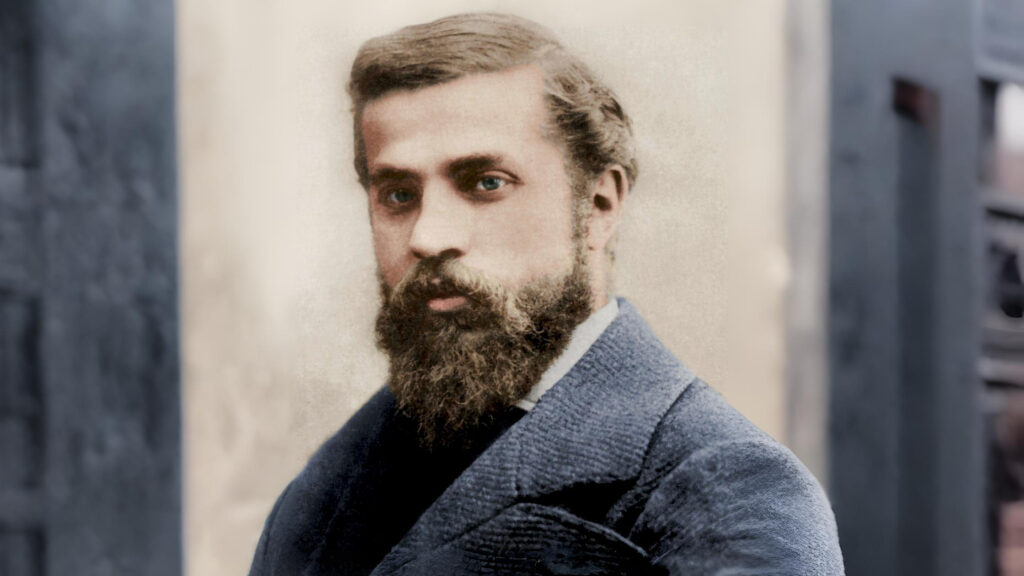
Antoni Gaudí Takes Another Step Toward the Altar: Declared Venerable by the Church
Exaudi Staff
14 April, 2025
2 min
 (EN)
(EN)
 (ES)
(ES)
 (IT)
(IT)

